Abstract
Background: Hematopoietic cell transplantation associated thrombotic microangiopathy (TA-TMA) is an increasingly recognized complication and is associated with higher non-relapse mortality in allogeneic transplant (HCT) patients. Recent studies have indicated an association between complement activation of the terminal pathway (sC5b-9) and TA-TMA, leading to the utilization of complement blockade as a means for therapeutic intervention in cases of TA-TMA (Jodele, 2016, Bohl 2017). It is unknown, however, whether complement activation routinely occurs in the inflammatory milieu after transplant and whether such activation is associated with clinical outcomes. Therefore, we conducted a prospective analysis of complement activation from plasma samples drawn from HCT patients. We hypothesized that complement activation is associated with subsequent development of clinically relevant outcomes such as TA-TMA or aGVHD.
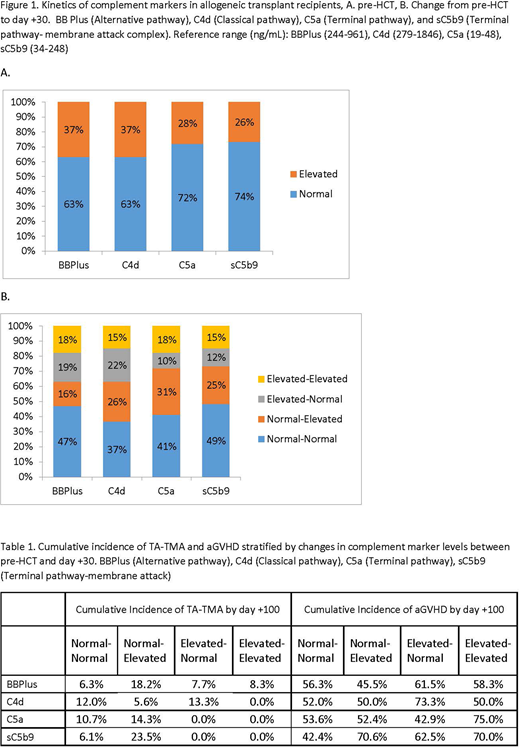
Methods: We performed a prospective analysis of complement activation in 76 patients who underwent hematopoietic cell transplantation and reached day +90 between January 2017 and June 2018. Plasma samples were collected from patients at admission for the Pre-HCT timepoint, and subsequent samples were collected at day +30 (± 7 days). Complement markers included C5a (Terminal pathway), sC5b-9 (terminal pathway - membrane attack complex), C4d (Classical pathway), and BB Plus (Alternative pathway) were measured as previously described (Yang 2015). Following enrollment, transplant-related demographic data was collected, as well as any new cases or flares of aGVHD and/or TA-TMA, and patient survival. Changes in complement markers from pre-HCT to day +30 were categorized into four groups: 1. Normal - normal 2. Normal - elevated 3. Elevated - normal 4. Elevated - elevated. Time to TA-TMA was defined as days from transplantation to TA-TMA onset censoring those without TA-TMA at last follow up date, treating death as a competing risk. The cumulative incidence rate of TA-TMA was estimated and the Fine and Gray regression models accounting for competing risk were used to examine the association between change in complement markers and risk of TA-TMA. aGVHD was similarly analyzed. OS was defined from the date of transplantation to the date of death, censoring those alive at the last follow up date. Cox proportional hazard models were used to evaluate the associations with risk of death.
Results: The median patient age at the time of transplant was 60 years (19-72) and 36.8% were female. Reduced-intensity conditioning was used in 76% of the patients and 58 of the 76 patients received tacrolimus as GVHD prophylaxis. Of the 76 patients, the cumulative incidence of aGVHD by Day 100 was 55.3% (95% Confidence Interval (CI): 43.4-65.6%) and the cumulative incidence rate of TA-TMA by Day 200 was 14.2% (95% CI: 7.2-23.5%). Median duration of follow-up was 270 days and overall survival was 81.4% by day +365.
Complement Activation, TA-TMA, aGVHD, and Survival: At the pre-HCT time point, more than 25% of patients had evidence of complement activation (Figure 1A). However, pre-HCT complement activation was not associated with subsequent TA-TMA, aGVHD, or overall survival. We then evaluated changes in complement activation from pre-HCT to day +30 and correlated with incidence of aGVHD and TA-TMA (Figure 1B, Table 1). When compared to normal - normal group, patients in the normal-elevated sC5b-9 group had a higher risk of subsequent TA-TMA (Hazard Ratio (HR): 13.4, 95% CI: 1.6-109.9, p=0.02), and patients in the elevated - elevated C5a group had a higher risk of developing aGVHD (HR: 2.8, 95% CI: 1.01-7.6, p=0.049).
Discussion: We show that complement activation can occur pre-HCT and is dynamic post-transplant. However complement activation pre-HCT does not correlate with clinical outcomes. Changes in terminal complement pathway between pre-HCT and day +30 correlate with subsequent development of TA-TMA or aGVHD. These results suggest that kinetics of complement activation may indicate a role of this pathway as a biomarker in diagnosis of TA-TMA and aGVHD. Further evaluation is necessary to explore whether complement inhibition might be effective as a therapeutic approach in aGVHD and TA-TMA.
Cataland:Ablynx: Consultancy, Other: Member of Advisory Board; Shire: Consultancy; Alexion: Research Funding. Vasu:Boehringer Ingelheim Inc: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal